

Undoubtedly, the fast, objective, and noninvasive OCT has emerged into a valuable tool, not only in DME, but also in other macular diseases such as age-related macular degeneration (AMD) and central serous chorioretinopathy. In the past decade, the evaluation of treatment efficacy was mainly based on visual acuity measurements and the detection of structural improvement on optical coherence tomography (OCT) scans. Treatment of diabetic macular edema is readily available and management guidelines of diabetic macular edema have largely evolved around the use of new laser machines, newer pharmacological agents such as antivascular endothelial growth factors (anti-VEGF), and different steroid preparations. Diabetic macular edema (DME), being a complication of diabetes, is an important cause of visual loss in developed countries. Introductionĭiabetes mellitus is one of the commonest chronic diseases affecting all populations especially developed countries. Moreover, it could be a potential long term visual prognostic factor for patients with DME. It is a novel OCT parameter in the assessment of DME. ORL thickness correlates better with vision than the total retinal thickness. The correlation coefficient between total retinal thickness and visual acuity was 0.34 ( P < 0.001) whereas the correlation coefficient was 0.65 between ORL thickness and visual acuity ( P < 0.001). The mean age was 58.1 years (☑1.5 years) and their mean visual acuity measured with Snellen chart wasĠ.51 (☐.18). Results.ħ8 patients with DME were recruited. The correlation between total retinal thickness, ORL thickness, and vision was calculated.
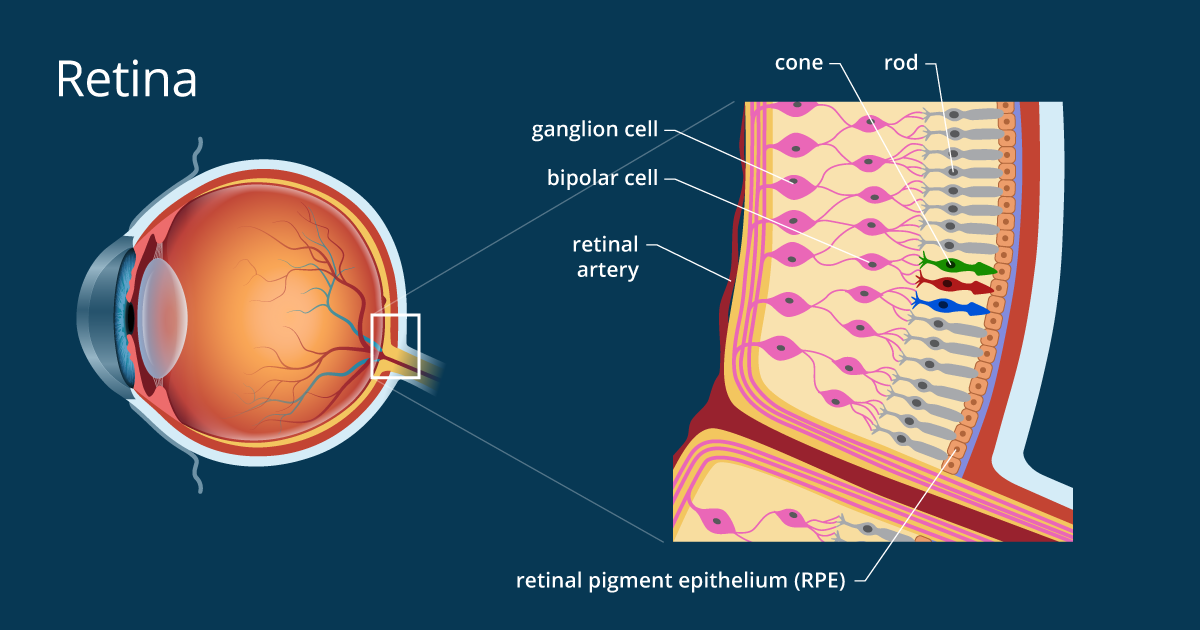
The ORL thickness was defined as the distance between external limiting membrane (ELM) and retinal pigment epithelium (RPE)Īt the foveal center. Retina Clinic of The University of Hong Kong were recruited for OCT assessment. In patients with diabetic macular edema (DME). To investigate the correlation of outer retinal layers (ORL) thickness and visual acuity (VA)


 0 kommentar(er)
0 kommentar(er)
